Lawmakers push health care cost-saving, price-transparency bills forward
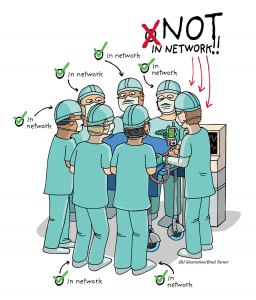
The measures are largely focused on ending surprise billing for patients, creating an all-payer claims database and requiring health care providers to give patients costs estimates in advance.