Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe Now
It’s that time of year again, when benefits managers are calling employees together in a conference room or auditorium and dishing out the tough news: The cost of health care is going up. Again.
As open-enrollment season approaches, Indiana benefits consultants are predicting that employer-sponsored health insurance plans could rise in cost at many companies by double digits, driven by inflationary pressures and the higher cost of many prescription drugs that treat cancer, psoriasis, diabetes and other disease areas.
That would continue the upward cost increase in health benefits that for years has shrunken employee paychecks and eaten into the bottom line of companies.
The issue looms large for Indiana, where employer-sponsored plans covered 52.1% of the population as of 2022, higher than all neighboring states but Illinois, according to San Francisco-based research firm Kaiser Family Foundation.
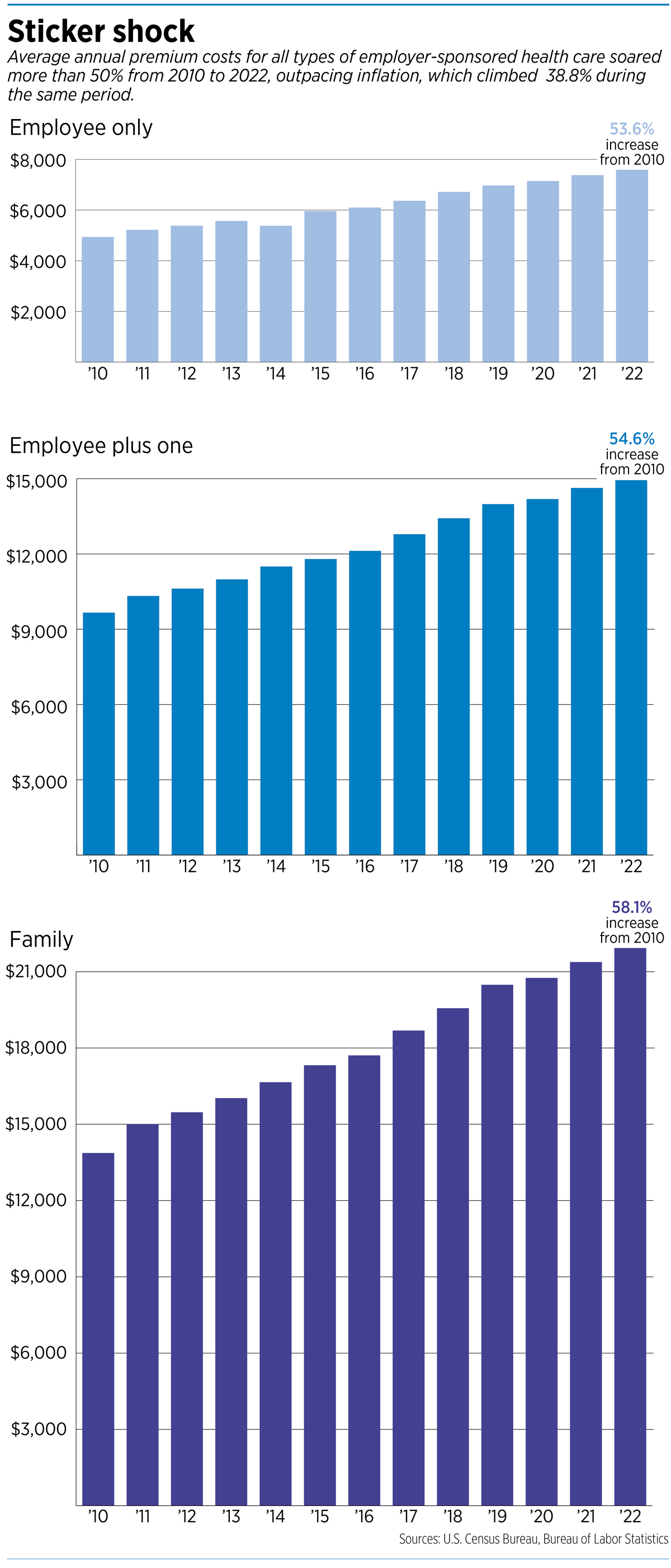
The average family premiums for employer-sponsored health insurance soared 58% from 2010 to 2022, while wages grew 29% and inflation climbed 39%, according to the U.S. Census Bureau and the Bureau of Labor Statistics.
Nationally, the average cost of employer-sponsored health plans is expected to grow 9% next year if companies don’t find ways to cut costs, according to an Aug. 15 report by professional services firm Aon.
“Medical claims continue to trend at elevated levels, while prescription drug costs are climbing higher due to continued growth in specialty drugs and increased utilization of GLP-1 medication for diabetes and obesity,” the report said.
The huge demand for GLP-1 drugs, including Indianapolis-based Eli Lilly and Co.’s diabetes treatment Mounjaro and obesity treatment Zepbound, temporarily caused shortages for millions of patients. The drugs can cost more than $10,000 a year, although Lilly announced last month it is now selling vials of Zepbound for about half of the usual monthly price.
New York City-based PwC, one of the Big Four accounting and consulting firms, is estimating an 8% increase in the overall cost to treat patients next year in the group market and said those increases will be shifted to employers and employees.
“Innovation in prescription drugs for chronic conditions and increasing use of behavioral health services are reaching a tipping point that will likely drive further cost inflation,” PwC’s Health Research Institute said in its July 19 report.
And in what might seem like pouring salt into a wound, the report continued: “Employers may need to make difficult decisions regarding benefit offerings and cost-sharing arrangements.”
That might include making decisions about which drugs to include in benefit formularies and possibly drawing narrower networks of providers, including hospitals, medical clinics, and outpatient labs and imaging centers.
A recent survey by the consulting firm Mercer found that 45% of employers were likely or very likely to shift rising expenses onto their employees.
But that could make it harder for workers to pay for health care—and would likely lead to long faces in the conference room if a company rolls out a plan to have workers pick up even more of the cost. About 43% of people with employer-sponsored coverage said it is difficult to afford care, according to a survey published last year by the Commonwealth Fund.
Since 2010, the share of premiums that employees bear has remained relatively constant: about 20% for single coverage and 32% for family coverage, according to the Bureau of Labor Statistics. Employers pay the remainder of the premium cost.
A strain
The Kaiser Family Foundation didn’t pussyfoot around the issue in a report it issued in May. “Ultimately, health care is expensive, and the cost of good [employer-sponsored insurance] coverage can place a strain on employers and employees,” the organization said, “particularly for workers with lower wages.”
In Indiana, health consultants and brokers say they are expecting premiums to increase by a wide range, depending on numerous factors, but say companies and employees shouldn’t be surprised by an increase of 10% or more.
Most of the health insurance purchased in Indiana is through so-called “self-funded” group plans, which means a company bears the risk of really large claims. Therefore, many self-funded employers buy stop-loss insurance from so-called “reinsurers” that kick in for large, one-time bills or when overall claims reach a high threshold.

At Apex Benefits, an Indianapolis-based benefits consulting firm, officials say reinsurance carriers have been starting to lose money from numerous large claims.
“So I would anticipate some of their increases are going to be more in the 12% to 15% range,” said Stan Jackson, Apex’s chief innovation officer. “And if you’ve really had a bad year, with lots of ongoing claims, you can expect to see something much higher than that.”
Chad Morris, vice president at Gregory & Appel, an Indianapolis-based benefits firm, said he is seeing 2025 health insurance costs range from small reductions to upwards of 10%. “If you’ve got a really, really bad situation, like a high-cost claims situation going in a self-funded plan, then you might be even in the 15-plus-percent range,” he said.
He said the severity of claims is rising in Indiana, often involving million-dollar claims. “There are more million-dollar claims than there have ever been before,” Morris said. “And so, if an employer-sponsored plan has one of those claimants on their plan, it can be tough to maneuver.”

Marcus Bowing, a partner at LHD Benefits Advisors in Indianapolis, said large institutional employers, those with 1,000 employees or more, are seeing increases in the 5% to 8% range. Companies working to reduce risks and tighten costs will usually get better prices, he said.
“You have to really think about, where are people going for their primary care and specialty care?” Bowling said. “And is that the most expensive hospital system in our state?”
High Indiana costs
That’s emerging as a huge issue in Indiana, where hospital prices remain among the highest in the nation, according to the latest study by California-based research group Rand Corp., released in May.
Indiana employers and employees are paying nearly three times, or 297%, what Medicare pays for the same services at the same hospital, the study concluded. That’s higher than the national average (254%), and higher than neighboring states Michigan (192%), Kentucky (231%), Illinois (247%) and Ohio (277%).
Overall, Indiana’s total commercial hospital prices are eighth-highest in the country, a slight improvement from the last study, when Indiana was seventh, the study found.
In response, the Indiana Hospital Association has said Indiana physicians are among the lowest-paid in the nation. Therefore, hospitals subsidize physicians at a high level, which makes Indiana hospital prices “look artificially higher than other states.”
It’s a debate that’s sure to continue even into the 2025 session of the Indiana General Assembly, which has been studying the cost of health care and promising relief to patients and employers for several years.
So-called “fully funded” health insurance plans can be more expensive than self-funded options, but they can also offer more financial predictability and be a more attractive benefit option to employees, according to PeopleKeep, a developer of health-benefits software.
Nationally, 164.7 million people relied on employment-sponsored health insurance in 2023, more than any other type of coverage, including Medicare, Medicaid and individually purchased insurance on the Affordable Care Act exchanges.
Employers help shield workers from much of the cost of their health insurance premiums, although employees often feel the impact via smaller take-home pay and higher deductibles and copayments.
Crucial to compensation
If there’s a silver lining in all the numbing news about higher health care costs, it might be this: Most employers will not cut health benefits, and many will make enhancements to their programs, although they might be doing so more selectively than in past years.
That’s important to employees, because health insurance is one of the main benefits employees look for when considering a firm’s compensation package, according to the Center for American Progress, a left-leaning public-policy research and advocacy organization.
“Offering robust health insurance is an important recruitment and retention tool for employees, especially considering the high levels of employee attrition in 2021 and 2022,” the organization wrote in a white paper in 2022 under the headline “Health Insurance Costs are Squeezing Workers and Employers.”
Health insurance is second only to wages as part of employee compensation. One factor that drove employer-sponsored insurance to prominence in the U.S. health care system was World War II-era laws that excluded health insurance from wartime wage controls, the Center for American Progress report said.
“The endurance of [employer-sponsored insurance] is bolstered by the tax exemption for health insurance premiums,” the report said. “Employer contributions toward premiums are exempt from income and payroll taxes, and employee contributions are generally income tax exempt.”
Yet the rise in modern medicine and drug development has pushed the cost of health care up for employers and employees alike.
New, specialty drugs for everything from rheumatoid arthritis and plaque psoriasis to cancer and Alzheimer’s disease might be terrific for patients but come at a cost to many employer groups.
“All these specialty drugs keep coming out, many at $50,000 or $60,000 a year,” Jackson said. “They bring relief to people, but there’s a financial cost to those drugs as well.”•
Please enable JavaScript to view this content.

Neither political party at any level has any answers to reduce healthcare costs or improve the system. All talk. No action!!!
How much of the healthcare dollar goes to the Health Benefit Brokers who ration the services? My bet is that it is significant, in the 10-20% range, and growing, and neither those in need of care nor the caregivers are happy with the results.
There are more cost effective treatments, even cures, in other developed countries which aren’t allowed in US. Without tackling Big Pharma and rotating door between gvmt agencies and pharma, there’s no answer to utilizing these options or slowing soaring prescription costs. Not a partisan issue as both parties benefit greatly from pharma. Big Pharma is so entrenched in the FDA, NIH, and Capitol Hill that it’s almost untouchable except for a select few that Medicare has singled out.
https://www.msn.com/en-us/money/markets/nih-scientists-made-710m-in-royalties-from-drug-makers-a-fact-they-tried-to-hide/ar-BB1nuldg
https://www.forbes.com/sites/johnlamattina/2022/09/22/why-is-biopharma-paying-75-of-the-fdas-drug-division-budget/
https://www.statnews.com/feature/prescription-politics/federal-full-data-set/