Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe Now
It was the shot heard around the medical world.
Last month, the federal Medicare program proposed a 2.9% cut to physician pay for 2025. That marked the fifth straight year that regulators proposed cutting payments to doctors for thousands of services, from stitching a wound to replacing a knee, even as the costs of supplies, labor and other expenses continue to rise.
Many physicians say Medicare patients make up 30% to 50% of their practice, and they’re calling on Congress to prevent the payment cuts from going into effect next year.

Physicians and practice administrators across Indiana decried the proposed cuts in interviews with IBJ, pointing out they’ve been forced to absorb higher costs of running a practice while Medicare wants to keep cutting payments.
As Dr. David R. Diaz, an Indianapolis psychiatrist, sees it: “You kind of get tired of getting kicked when you’re down.”
Dr. William Pond, a Fort Wayne anesthesiologist, said it gets harder for practices to survive when revenue gets closer to the break-even point. “And I think that’s what we’re getting to,” he said.
And as far as Steve Freeland, CEO of the Cancer Care Group in Indianapolis, is concerned, Medicare “is dismantling the very existence of independent practice physicians, whether intentional or not.”
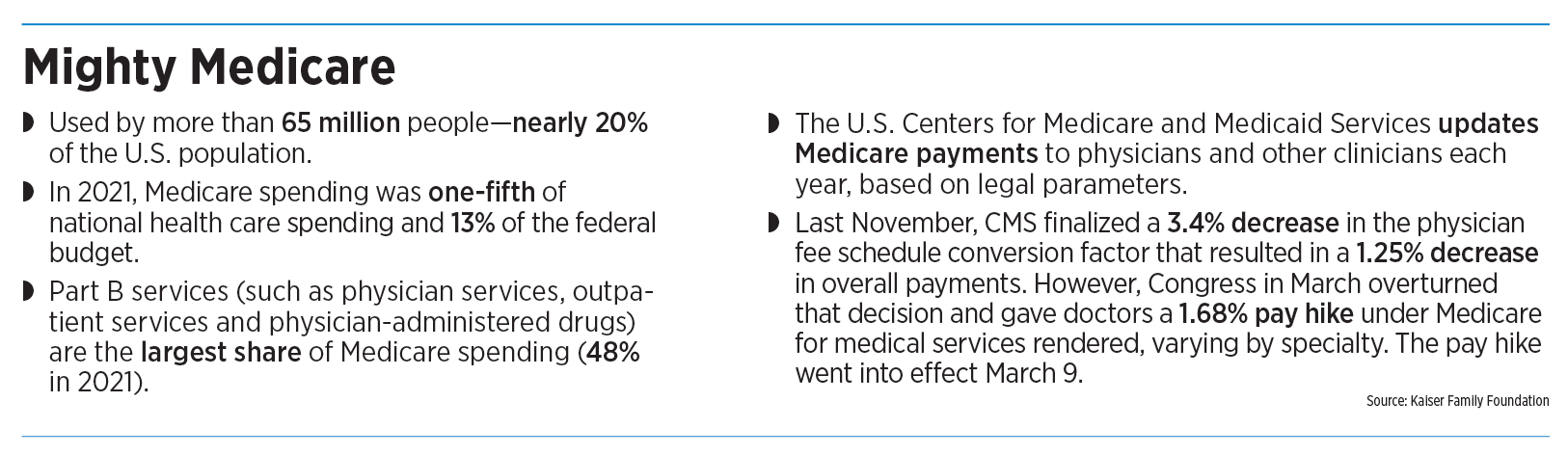
More than 65 million people, nearly 20% of the U.S. population, receive health insurance coverage through Medicare, according to the Kaiser Family Foundation.

The U.S. Centers for Medicare and Medicaid Services updates Medicare payments to physicians and other clinicians each year based on certain metrics.
Lately, the regulators have been updating in one direction: cuts in physicians.
“The death by a thousand cuts continues,” said Dr. Bruce A. Scott, president of the Chicago-based American Medical Association, in a written statement.
Yet Congress can step in and overturn Medicare’s rules, as it did this past March, when it gave doctors a 1.68% pay hike for services this year, varying by specialty, even as Medicare wanted a cut of about 1.25%.
Other medical groups, including the Medical Group Management Association and the American Hospital Association, also oppose payment cuts to doctors. But some physicians say they don’t have the clout to match the power of a huge government program.

“We’re an easy target,” said Dr. Ed Hellman, an orthopedic surgeon and president of OrthoIndy, a physician-owned medical practice and hospital based on the northwest side of Indianapolis. “You know, people think the AMA is very powerful. But physicians’ lobbies traditionally have been very disparate and not particularly well organized.”
Losing independence
The federal government’s move is the latest squeeze on physicians, who have increasingly seen their expenses grow while struggling to keep their practices running. From 2012 to 2022, the share of U.S. physicians who were self-employed fell from 53.2% to 44%, according to the American Medical Association.
In contrast, the share of physicians who were employed by hospitals, medical clinics and other organizations grew from 41.8% to 49.7% during the same period.
Physicians in Indiana already rank third-lowest in the nation for prices paid by commercial insurers, according to a 2022 report by the Congressional Budget Office, based on 2018 data.
“Proposed federal cuts to physician reimbursement are deeply concerning, especially in Indiana, where physician rates set by commercial insurance companies are near the lowest in the country,” the Indiana Hospital Association said in a statement. “Because of these low rates, Indiana hospitals subsidize physician payment at great expense to preserve access and keep physicians in the community.”
The association warned that continued cuts by Medicare would “exacerbate financial challenges” in the health care system and further shift the cost onto employer-sponsored health plans.
Medicare officials have said the cuts were necessary to comply with a federal law that requires the programs’ physician compensation to remain “budget neutral.” Each year, the Centers for Medicare and Medicaid Services updates Medicare payments to physicians through rulemaking, based on parameters established under law.

“Like every other federal agency, they’ve got a budget and a fiscal master,” said David Blish, director of health care consulting for Katz Sapper & Miller, an Indianapolis-based accounting and consulting firm.
Last year, Medicare finalized a 3.4% decrease in the physician fee schedule “conversion factor,” a key aspect of Medicare payment rates. That resulted in a 1.25% decrease in overall payments— depending on medical specialty—before Congress overturned the decision.
The rulemaking process is complex and uses a “conversion factor” to convert what’s known as “relative value units” into payments. The relative value units are measurements of the relative economic value of medical care, based on factors like a physician’s time, skill and training; professional liability; and cost of supplies, staff, equipment and building space.
When Medicare adds reimbursement for more services or the cost of services increases, it has to lower the conversion factor to prevent a net increase in costs to the federal government.
‘Not all negative’
Blish said that even as the Medicare physician payment rate is falling, there’s some good news for physicians. The federal agency is adding ways for physicians to expand billing, such as allowing physicians frequent visits with chronic-care patients.
“CMS is trying to expand the way physicians can bill and code their time and get adequately reimbursed. So it’s not all negative,” he said.
Even though Congress has prevented the worst of the reductions from going into effect, as far as some Indiana doctors are concerned, the frequent cuts can add up.
Diaz, the Indianapolis psychiatrist, said Medicare today pays doctors 29% less, adjusted for inflation, than in 2001. He said many physicians are suffering from burnout, and the Medicare payment cuts are not helping.
“It doesn’t feel good to help people through COVID and then get rewarded with a pay cut from Medicare,” said Diaz, who is also president of the Indiana State Medical Association, which represents more than 9,000 physicians and medical students.
He said the cuts have prompted some doctors to stop accepting new Medicare patients because they can’t afford to take lower reimbursement rates and keep their doors open.
He said few patients likely realize that many doctors are taking pay cuts from Medicare, even as they have to pay more for supplies, rent, equipment and labor. He acknowledged that he is “well compensated” as a physician who works for Indiana University Health, the state’s largest hospital system. But he declined to disclose his compensation.
“I’m not a prima donna and think that I should be handed money because of past efforts,” Diaz said. “I may stay in practice for another four or five years. But this [cut in Medicare payments] is just another straw that eventually will break the camel’s back.”
IU Health spokeswoman Lisa Tellus told IBJ that its physicians are employed under contract and won’t see their salaries cut when outside payers such as Medicare reduce their payments for physician services.

Other large hospital systems in central Indiana, including Community Health, Ascension St. Vincent and Franciscan Health, did not respond to IBJ’s questions about Medicare cuts.
Deaconess Health System in Evansville said it employs a “fairly significant number of physicians,” and that almost all of its doctors are employed under an arrangement through which their compensation isn’t directly impacted by Medicare reimbursement.
But Indiana has an undersupply of doctors, and health care systems are under pressure to keep enough on staff, said Dr. James Porter, president of Deaconess’ physician division.
“And so there’s a lot of competition, especially for certain specialties, in order to attract them to a region and have adequate access to those physician services,” he said.
No new patients?

Some independent physicians say they are loath to turn away patients, including those on Medicare, but that doesn’t stop the financial squeeze at their practice. Dr. Cindy Basinski, a urogynecologist in private practice in Evansville with one other physician and seven employees, said the majority of her patients are on Medicare and often need expensive procedures common to women in their 50s and 60s.
“A lot of practices won’t take on more Medicare,” Basinski said. “I won’t turn anyone away.”
That’s even as she has had to give raises to all her employees, pay the higher cost of supplies and employee health insurance, and face other cost increases.
Some practice administrators see a dire landscape. “Millions of seniors will find it more difficult to access high-quality care, and physicians will find it difficult to accept new Medicare patients,” said Angie Stevenson, CEO of Indiana Hand to Shoulder Center, an orthopedic practice in Indianapolis.

“It’s not rocket science to understand that, if your expenses keep going up and reimbursement keeps going down, you reach a point where you can’t stay in practice,” said Dr. Francis Price, an ophthalmologist in private practice in Indianapolis.
The Cancer Care Group, an independent practice of 20 radiation oncologists based in Indianapolis, said the Medicare cuts are the “kiss of death” for private-practice physicians. That’s unless the cuts are offset by increased rates paid by commercial health plans, which then often translates to increased health care premiums for employers and employees, said Freeland, the group’s CEO.
Pond, the Fort Wayne anesthesiologist, said the big question for independent practices is whether to accept more Medicare patients and, if so, how many.
“They have to decide whether they’re going to do that or limit it to existing Medicare patients or limit the number they will do per day,” said Pond, the president-elect of the Indiana State Medical Association.
“There’s a certain point at when, if your patient mix becomes very high in Medicare or Medicaid, and you don’t have enough revenue coming in to meet your expenses,” he said. “And then you have tough choices to make.”•
Please enable JavaScript to view this content.