Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe NowAt Franciscan Health’s Indianapolis hospital, the number of people being treated for COVID-19 shot up this week to about 40, double the number from just a month ago.
At Reid Health in Richmond, the surge of COVID-19 patients has gotten so severe that doctors have stopped accepting referrals from nearby hospitals and have started looking for ways to discharge other patients earlier than normal.
And at Lutheran Hospital in Fort Wayne, officials are wondering if COVID-19 patients could soon fill many of the hospital’s 396 beds.
“We might get 20 patients today, 20 tomorrow, and 20 more the day after that,” said Dr. Vishal Bhatia, the hospital’s chief medical officer. “And if they keep on increasing, what do we do? There is a finite point to everything.”
Across Indiana, the number of COVID-19 hospitalizations has been shattering records day after day, putting a strain on many hospitals and adding to the anxiety about how much longer the pandemic will continue.
The Indiana Hospital Association issued an unusually blunt warning this week, saying that medical facilities are struggling to keep up with patient loads.
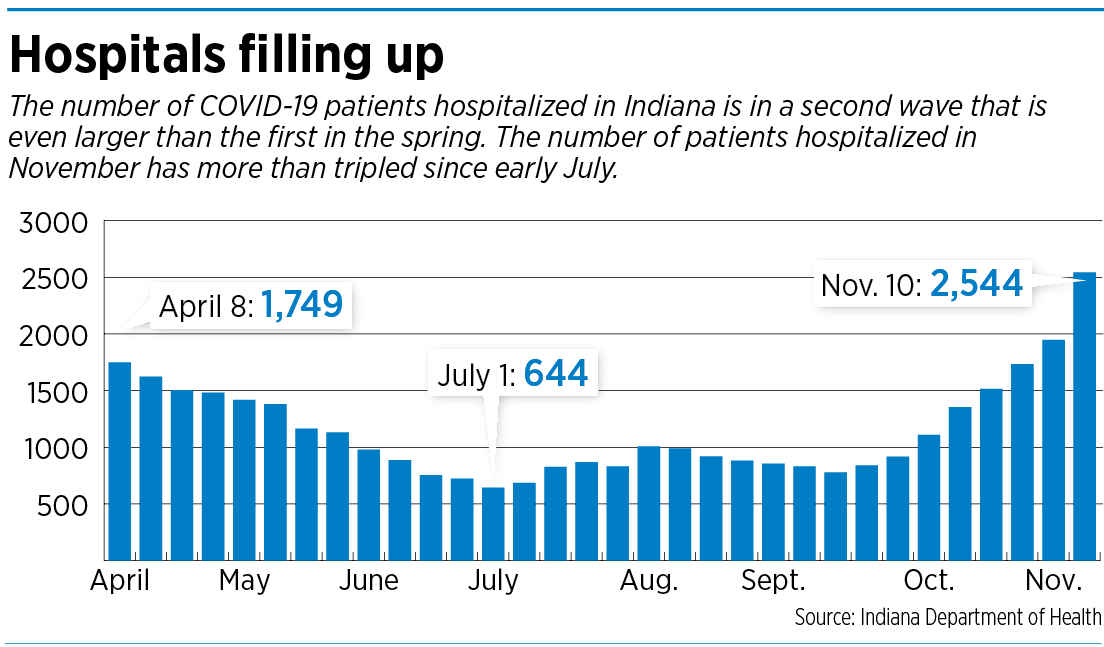
It pointed out that hospitalizations across the state from COVID-19 have increased 143% since Oct. 1, and called on people to wear face coverings and practice social distancing. After hovering in triple digits for the past five months, hospitalizations stood at 2,544 as of Wednesday.
“All Hoosiers should be alarmed at the COVID-19 trends we are seeing across the state,” the hospital association said in a statement.
Straining resources
Indiana ranks eighth-highest among all states for hospitalizations on a per-capita basis, according to the COVID-19 Tracking Report, a volunteer organization launched by The Atlantic to collect and publish data on outbreaks.
Nationally, more than 62,000 people were hospitalized with COVID-19 on Tuesday, up 40% in just two weeks, and the most the country has ever seen, the report said.
The number of Hoosiers hospitalized for COVID-19 broke through the 2,000 mark last weekend, after closing September at 919.
State Health Commissioner Dr. Kris Box said some hospitals are canceling or changing surgeries and other procedures to make sure they have the beds and staff they need to take care of patients.
The crush in hospitalizations in Indiana comes after the state lifted almost all pandemic-related restrictions on social gatherings and business activity in September. Gov. Eric Holcomb has told Hoosiers to wear masks and practice social distancing, but there are no penalties for not complying.
On Wednesday, Holcomb announced a new set of restrictions, effective Nov. 15, that would limit social gatherings to 25 people for counties with the highest rates of infection (coded red) and 50 people for those counties with the next-to-highest rate of infection (coded orange).
“This virus is unrelenting and will only gain momentum,” Holcomb said.
COVID-19 cases are surging in nearly every region of Indiana, with the northern region recording the highest number of cases, along with Marion County and portions of southern Indiana, the hospital association said. Most counties across the state are coded orange at this time, meaning the positivity rate in those counties has grown to a range of 10.0% to 14.9% in the last seven days.
“Many hospitals are reporting staff shortages as the pandemic takes its toll,” Brian Tabor, CEO of the Indiana Hospital Association, said in a statement.
 “Hoosier nurses, doctors and other front-line hospital staff have been working non-stop since the early spring. Please give these courageous health care heroes some much-needed relief by wearing a face covering, practicing social distancing, washing your hands, and staying home when you are sick. We need everyone to take these steps to relieve the enormous strain on the system at this critical time.”
“Hoosier nurses, doctors and other front-line hospital staff have been working non-stop since the early spring. Please give these courageous health care heroes some much-needed relief by wearing a face covering, practicing social distancing, washing your hands, and staying home when you are sick. We need everyone to take these steps to relieve the enormous strain on the system at this critical time.”
Several Indiana hospitals say COVID-19 patients fill less than 20% of their beds, but the number is changing by the day, and can climb by double-digit percentages in just a couple of weeks.
Testing the limits
Experts say there’s no magic formula for determining how much of an increase in patient load is too much. Hospitals that are near capacity often can’t tolerate even a 10% increase in patients, while hospitals that are half empty can easily deal with that increase, said Eugene Litvak, CEO of the Institute for Healthcare Optimization, based in Newton, Massachusetts, which helps advise hospitals on how to manage their capacity.
“It could be 5%, 10% or 30%,” Litvak said. “It depends on the hospital.”

Franciscan Health is seeing “a significant uptick in inpatient COVID patients,” and is nearing an all-time high in hospitalizations, said Dr. Christopher Doehring, vice president of medical affairs.
But the issue goes beyond raw numbers, he said. COVID-19 patients typically require at least a week of hospitalization and sometimes much longer, he said, compared with the average inpatient stay of about five days.
“So, you can see if the number of these COVID patients keeps going up, it has kind of a compounding effect on hospital capacity, because of that longer length of stay,” Doehring said.
Goshen Health in Elkhart County reported 44 patients on its COVID-19 unit this week, a record, accounting for nearly half of the hospital’s 107 staffed beds.
“Some patients who need important surgeries are having their procedures delayed because COVID-19 patients are filling our intensive care unit beds,” Dr. Dan Nafziger, chief medical officer at Goshen Health, said in statement. “We’ve had to transfer some patients because we didn’t have enough beds.”
At nearby Elkhart General Hospital, about 92 patients this week, or about half of the census, are COVID-19 patients, and the hospital on Tuesday had to divert ambulance traffic, according to TheGoshen News.
“We don’t have any other place to put our patients,” Dr. Michelle Bache, vice president of medical affairs at Elkhart General told the newspaper.
Preparing for onslaught

Some Indiana hospitals began adding capacity or dedicated units for COVID-19 patients earlier this year, when the first wave was occurring, to avoid becoming overwhelmed.
Over the summer, Hancock Health set up a dedicated unit with 60 beds and oxygen units on the second floor of its new medical clinic off of Interstate 70’s Mount Comfort Road exit, about 10 miles west of its Greenfield hospital. The unit is for patients who need hospital care, but don’t require intensive care or ventilation.
“So we have quite a bit of ability, with a separate oxygen utilization, should we need to go there,” said Dr. Julia Compton, CEO of Hancock Physician Network.
Even in hospitals that have only admitted a handful of COVID-19 patients, officials are concerned the numbers might spike, especially as the weather turns colder and people begin to gather indoors for holidays gatherings.
Johnson Memorial Health has fewer than a dozen COVID-19 patients under its roof most days, and with 65 staffed beds, things are manageable for now, said Dr. David Dunkle, the system’s CEO. But that could change with little warning.

“I’m not going to lie to you,” Dunkle said. “I’m worried.”

Staffing challenges
It’s hard to know which hospitals are feeling the biggest squeeze. The Indiana Department of Health lists the total number of hospitalizations and admissions statewide, with daily updates, on its web dashboard. But it does not break down the information by region, county or hospital. It also keeps a running tally on the percentage of intensive care beds and ventilators available.
As of Tuesday, 30% of ICU beds were available across Indiana, a 23% decrease compared to Oct. 1. The number of available ventilators remained high, at 77%.
That said, each hospital has surge capacity that it can access to handle larger influxes of patients, the state hospital association said. Early in the pandemic, Indiana hospitals were able to double ICU capacity.

In central Indiana, the large hospital systems say they still have plenty of beds and are not afraid of hitting capacity in the near future. They say the crunch is not about beds, but whether they have enough medical and nursing staff to tend to patients. Hospitals have been hit hard with staff members who have been forced to quarantine or isolate after getting infected or being close to someone who had the virus.
“We have the beds. Staffing is the issue,” said Dr. Robin Ledyard, chief medical officer of Community Health Network.
She said the Indianapolis-based system has been admitting three to five people every day for the past week, and now has 81 positive cases at its six hospitals, along with 25 people admitted who are awaiting testing results.
But while the number of patients at Community Health is climbing, staffing levels are not keeping pace. As of last week, about 160 of the system’s 16,000 workers were quarantined or isolated after getting infected or spending time with someone who later tested positive.
At Indiana University Health, the state’s largest hospital system with 16 hospitals, about 700 staff members are now under quarantine and unable to work—a sizeable slice of the system’s workforce of about 35,000.

The decrease is causing problems in various units, said Dr. Michele Saysana, chief quality and safety officer. “When you start to get down to unit levels, if you’re trying to staff units, and you have even four or five people calling in, that creates a big challenge.”
The problem is not yet so severe that IU Health has had to cancel any elective surgeries, she said.
Box, the state health commissioner, said last week that hospitals and health care workers in Indiana are “needing support now more than ever.”
Earlier this year, the state began recruiting retired and out-of-work health workers as part of a “health care reserve workforce” to help relieve staff shortages at hospitals and nursing homes. But the reserve workforce has been overwhelmed with requests in recent weeks and has told hospitals it can’t guarantee any reinforcements.
In the meantime, Gov. Holcomb has activated the Indiana National Guard to help relieve overwhelmed workers at all of the state’s 534 nursing homes and senior communities.
Wide variations
Some Indiana hospitals say they are doing the best they can to cope with an onerous situation. At Reid Health, which operates a single acute-care hospital in Richmond, near the Ohio border, COVID-19 patient volumes have been climbing sharply, into the high 70s in recent days, making this wave even bigger than the original surge in March and April.

Feeding that is a steady stream of people visiting the emergency room with COVID-19 symptoms. Reid Health’s ER is now admitting as many as 70 people a day, many of them COVID-19 patients–up from 30 to 40 during normal times, said Dr. Thomas Huth, Reid’s vice president of medical affairs.
“The problem is, we don’t have 60 or 70 beds available most days. We started out today with five open beds,” he told IBJ in an interview Tuesday.
The only way to deal with sharp increase, he said is to “to add space creatively.” And one way to do that is to discharge certain patients more quickly than under normal circumstances—if they are up to recovering from home or another health setting.
Reid Health, the largest hospital in east-central Indiana, has also stopped taking referrals from hospitals in nearby counties.
But other hospitals say they have yet to feel anything like the squeeze at Reid Health.

Ascension Indiana, for example, said that while its COVID-19 hospitalizations are increasing, “the numbers that we’re seeing in the hospital aren’t going up as fast as the numbers you’re seeing in the state as a whole,” said Dr. Stephen Swinney, chief clinical officer of the Indianapolis-based system.
He said Ascension Indiana has the ability to flex its capacity to meet higher demand by bringing in extra nurses from clinics and administrative offices to help in the hospital as needed.
Riverview Hospital in Hamilton County said it has spent “considerable time” in the past 10 days refining its plans for another COVID-19 surge. So far, it has been able to handle all COVID-19 patients, without worrying about stretching its capacity.
“We did this in the spring and found that it kept us from being overwhelmed,” Dr. Eric Marcotte, chief medical officer, said in an email to IBJ. “With new treatments and ways to care for patients, these plans are simply being refined and improved.”•
Please enable JavaScript to view this content.


Seems that asymptomatic health care workers infected with Covid-19 could care for patients infected with Covid-19 just fine. It’s not like you get “double Covid.” If there is a medical reason for the health care worker not to come to work (e.g., they are feverish and don’t have the strength), that’s one thing. But, sending otherwise capable personnel home seems unnecessary. (Friend of ours did this. She cares for elderly in a residential setting. The elderly developed Covid and she got infected. She simply stayed there at the residential facility for the 14 day quarantine period, taking care of the residents. No need for a “healthy” care worker to spend their time in a hazmat suit caring for the elderly. And, there was no need for her to go home and watch TV when she could be fulfilling her vocation.) Now might be the time for a few creative solutions.
Maybe a good idea? But you have to admit you’re grasping for straws since this doesn’t slow down the spread. How about the usual boring stuff that “takes away your liberty”: wear a mask, socially distance, wash your hands, etc.
It is beyond belief that anyone in our local and State governments would allow this total disaster to continue unchecked. The State’s plan is too little and too late. The plan must be more aggressive and thorough. It is totally clear that the current administration does not have the internal medical expertise to make a decent plan to balance both health and the economy simultaneously. It appears that there is no group within our State that be willing to seriously confront the current administration to force it to make significant chances. Healthcare professionals, hospital systems, medical societies, etc. have been eerily silent.
Even though I have written the following many times before, the basics remain the same. The citizenry of our State have to get the message again and again and again, etc. (Remember how long it took to get people to wear seat belts!!!!!!!!!!! The same craziness against seat belts is being used to avoid masks. Many of the same mistakes were made during the 1918 pandemic as well. Too bad history seems to be avoided in our schools at all levels.)
New record numbers every day!!!! How many citizens are we going let get sick, and how many are we going let die? It really is as simple as that.
However, let me try to understand the logic of the State response to the surging pandemic: Stage 5 is okay. Our focus, per Dr. Box, is to increase the amount of healthcare staff and healthcare capacity to take care of the increasing number of sick people. Oh by the way, please wear you mask, pretty please!! (I love it when Health Commissioner, who recently got over COVID-19 episode, has only this to offer to curb the raging pandemic in our State.
As I have said before our State needs outside expertise (e.g. Dr. Anthony Fauci) to tell us citizens the REAL status of our State’s current plan to mitigate the pandemic of our State. The current “experts” from State outside of government (e.g. IU) have done little more than to create a bunch of numbers that are totally not understood by the common lay person.
There needs to a ground swell of outrage from the medical community (i.e. hospital, physicians, medical organizations, nursing organization, pharmacists, etc.) to force a change in how our State is handling the pandemic.
The State has the money to finance, through the Care ACT, to fund a more comprehensively plan to provide all the necessary tools (PPE, testing, contact tracing, etc.) to get the situation under control.
A responsible government would be able to balance the economy AND public health. Indiana appears not to be able to multi-task. A responsible State government would be able to do both. (As a small business owner, I have lost at least 50% of my income for the year. I know the financial consequences of the pandemic. It took months as the beginning to obtain the necessary amount of PPE to keep my employees and customers safe. I have been able to keep the staff intact as well. However, one does not know what the future will bring)
Hopefully, with the election over for the State, our local leaders will begin to multi-task. Frankly, I do not expect any progress. With the flu season beginning and with more indoor events, we need to expect that things are just going to get worse.
Everyone for our State should realize that our current situation was avoidable. Letting things get worse by this State’s administration is UNCONSCIONABLE and INDEFENSIBLE.
Everyone should re-watch the scene from “NETWORK” where Peter Finch gives a speech that still resonates today. Here is the YOUTUBE link:
https://www.youtube.com/watch?v=ZwMVMbmQBug
Kudos for your commitment to posting this every time!
I agree. Thank you, Phillip.
Refer to Article Two for the State’s leadership stance.
Hey! We’re #8! We’re #8! Indiana finally breaks into the Top 10 of something! Oops, it’s not a good thing, though. Hey Trumpsters, wear your masks! I guess it wasn’t just a hoax and would go away after the election since it was media hype. SHAME ON YOU!
Randy, there are more people than ever wearing masks so stop with the trumpeters crap. Numbers are still increasing even with the number of people wearing mask
Hey Rhea, I’ll stop with the Trumpsters crap just as soon as I see 90%+ of the people wearing a mask. You Trumpsters finally came around and now about 50% of you wear a mask. The problem is it has to be nearly everyone for this thing to work. Just yesterday, in a doctor’s waiting room, a Trumpster was wearing a mask until he took a phone call and dropped it completely down – as if you can’t talk on the phone with mask. I was 8 feet away, but there were adults with a toddler on their lap on both sides of him just 3 feet away. I politely asked if he’d please wear his mask and he decided to give me a dirty look and pulled it up over his mouth but not his nose. I was going to remind him about the proper way to wear a mask but thought he might be exercising his 2nd amendment rights.
I’m with Rhea. Everyone acts like masks are the ultimate barrier and almost everywhere I shop I rarely see someone without a mask. Numbers are still increasing so I don’t think masks are a panacea. Yes, I wear them when asked to, wash my hands and try to be careful, but this idea that masks are going to stop the spread, I just don’t agree with. Their has been a lot of scientific and medical professionals who have waffled on mask use. I saw an earlier interview with Fauci from March maybe where he said they may make people feel better, but are not effective. He’s obviously changed his stance. Can we also stop with Democrats care about people and the Republicans (Trumpsters) do not crap. Are you really that dense to put everyone in one of those two camps. Finally I will say that I went to an outdoor concert with several thousand not distanced people at the end of the summer and I was thinking the whole time if I’m going to get this virus this would be the place. It should have been a super spreader event, but it didn’t happen, yet I can probably go the grocery today and catch it so who knows.
Please stop trying to inject politics into this. It was sick when the left did it at the beginning. It is equally sick now. The virus is surging now because it is following the path of a virus. Back in April we projected it to surge in October. The surge is happening all over the world. And, please remember that the masks you’re so strongly advocating now are the same masks that the “experts” said were ineffective in March through June (when the governments issued stay-at-home orders). They have run side-by-side comparisons. When comparing the same number of people with Covid and without, 71% of those with Covid said they wore their masks “all the time” or “nearly all the time” and 74% of those without Covid said they wore their masks “all the time” or “nearly all the time.” Thus, the mask wearing did not make a difference. At some point, it becomes “security theater.” That said, I wash my hands thoroughly, use lots of hand sanitizer, and wear a mask. I encourage others to do so. I also recommend you wear safety glasses. Like any airborne virus, Covid can infect you through your eyes; that’s one of the reasons for the discussion about the number of times you touch your face. Try to be safe. But, also, please stop injecting politics. It’s unnecessary and counterproductive. And, don’t forget to enjoy each day. You never know when your time will be up.
Thank you.
Mask wearing only works when everyone wears them. Not 71%, but everyone. Businesses where mask wearing isn’t possible need to close. The fact of the matter is that we should have all restaurants and bars shut down minus takeout, with all of their employees and owners paid by the government until this ends. That is where the vast majority of the spread is coming from. Indiana refuses to make that information public, but plenty of states like Louisiana and California do. No reason to think Indiana’s spread would be any different.
Patrick, your theory is based on someone named “they”. 🙂 The reason politics got injected into this is because the orange one decided he’d lead the way by diminishing the seriousness from the get-go and led us down a path of politicizing wearing a mask, opening up too soon, etc. Some of us are merely pointing out the obvious problem with that since so many Trumpsters still believe his insanity and refuse common sense measures. As soon as you get your team on the right page, we’ll stop reminding you that politics got this ball rolling and politics is what is preventing us from getting it right. Just read all the criticism leveled against Holcomb and Hogsett and why we should just “let ‘er rip”.
You are citing a study incorrectly and turning it into misinformation about mask-wearing. If you read the entire study report instead of just the single paragraph you are citing, the study focused on whether or not dining and drinking at indoor establishments increased the risk of getting COVID-19. The key point was that dining and/or drinking required the individuals to remove or lower their masks while indoors. That is considered a high-risk activity and the study proved that is true. It did ask participants about their overall mask-wearing and found the outcomes you cited, but your conclusion misses the point of the study. The study found that if you engage in a high-risk activity even once, it doesn’t matter what your mask-wearing habits are the rest of the time–you’re going to get COVID-19. I’m really tired of individuals misusing information to further their political agenda–whatever happened to intellectual honesty? From a former Hoosier physician
Agree Patrick. Time to take the politics out of this discussion and look at this no differently than any other health crisis. Could you imagine if we acted this way with the flu every year. Republicans want everyone to get the flu and die yet Democrats stay home and try not to infect people. Pretty ridiculous, right.
this is interesting. Maybe google is wrong, which wouldn’t be the first time. According to google, there is 190 hospitals in Indiana. They state above there is a total of 2,544 people in hospitals in Indiana from Covid related issues. That is about 13 per hospital. Is that a big number? I don’t know.
No, but they want you to think it is for some reason. Almost all of those people will survive and go home. There is also a big difference between being in the hospital BECAUSE of COVID and being in the hospital WITH COVID. They both count as a COVID patient (so I’m told). People get sick this time of year. People spread germs. This is a virus. It’s not going anywhere. This spike was predicted. As Patrick referred to above, wearing a mask is not going to prevent you from getting COVID nor is it going to prevent you from spreading COVID. Phillip up there needs to get a grip. This was NOT unavoidable. He actually thinks government mandates can stop this virus. Hey Phil, people die everyday in car wrecks WEARING a seat belt. People still drive knowing the risk. If you can’t handle the risk, stay off the road. We live with a lot of viruses and diseases. We roll the dice every day. We’ve seen that locking things down is NOT the answer. It delays the inevitable. Enjoy life and be as clean and healthy as you can.
Charles H, I was just wondering when we were going to get some alternate version of reality. Being in the hospital “because of COVID” and being in the hospital “WITH COVID”, still puts you in the hospital when you otherwise would have been living your normal life, so I don’t see why you make the distinction. If it makes you feel better about your risky behavior then go right ahead.
So I assume you must be trying to contribute to the problem because you have proof that “wearing a mask is not going to prevent you from getting COVID nor is it going to prevent you from spreading COVID”? If you want to tell me that there are no studies that prove maks wearing is effective, that is because it is unethical to expose test subjects to a deadly disease. Please stay the heck away from me, my family, the stores we shop in, and the places we do business.
If we had a 67,000 people a day hospitalized from car wrecks, or 1500 people a day die from car wrecks, we would see a heck of lot of people scared to get into a car. That would be about equal to being hospitalized about every 50 days for every single Hoosier driver.
I agree most people seem to be wearing masks now although many incorrectly. However a vast group still refuses to socially distance be it in bars, parties, sporting events, etc. Look at all the complaints about the new restriction levels. The resistance to these measures is what burns me . . “if your scared stay home” they say. It’s mostly people who think they are healthier, younger, smarter, or better than the experts and everyone else or just don’t give a damn about anyone but themselves. A week in the hospital is the only thing that will cure those people of their ignorance and selfishness.. Why is it some people can be told you will get burned by fire and know it is true whereas others have to experience it to believe it. Nobody should complain about a potential shut down or worsening of this epidemic if they complain about masks, social distancing or restrictions put in place to try and prevent it.
It’s tough being smarter than everyone else. Smart people always have something to blame. You realize “Experts” can’t even agree on things. You have your “experts”. I have mine. So now we aren’t wearing our masks correctly or groups of people who don’t have COVID have the audacity to get within 6 fleet of each other. To my knowledge, none of the REALLY smart people (those people with Dr. in their title. I have a sister with one of those next to her name) have ever said we can “PREVENT” people from getting this virus so why do you think we can? The government mandates were enacted to “slow the spread” of the virus so our hospitals wouldn’t be over-run. Most smart people know that there is no cure for this virus, and like the flu, there likely won’t be. Like a snow ball rolling downhill, the more people who think they are smarter than everyone else keeps saying we can “PREVENT” the spread or “PREVENT” getting the virus, the more they say it, the more they think it’s true. Sorry, I’m one of the dumb people who think we will have to work our way through this and learn to live with some form of it. A vaccine will come that will help some people avoid contracting the virus but nobody will likely “PREVENT it”. Thank God the mortality rate is still very low. Straight from the CDC website….. “There is currently no vaccine to prevent coronavirus disease (COVID-19). You can take steps to slow the spread of COVID-19”. At what point do people get to decide when they can get on with life? Maybe between you, Phillip and the government…..you can let us know.
A Primer on Surviving COVID-19
As COVID-19 roars out of control, I thought it might be useful to summarize a WSJ article in Saturday’s issue on how to fight COVID-19. I hope President-elect Biden read the article as well, as it outlines where the Trump administration failed, both in terms of leadership and in terms of implementing effective measures to limit COVID-19.
There is no one measure that works in a pandemic, not lockdown, not masks, nor even vaccines. Instead, a variety of interventions must be simultaneously implemented to achieve what is called the “Swiss Cheese effect.” Like Swiss cheese, no intervention is perfect, each has various sized “holes” that allow the virus through. However, if you deploy enough simultaneous interventions (layers of Swiss cheese, laid on top of each other), the holes, of various sizes and in various locations, effectively block the path of the virus from getting through (see graphic).
The main non-pharmacological interventions available to us are behavioral in nature. They come in two broad categories: individual and collective.
Individual interventions include: washing hands, mask-wearing, avoiding face touching and self-isolation. Implementing these behaviors require individuals to take responsibility for their behavior. The goal is not only to protect the individual, but also those around them. These measures are not perfect and are not enough to protect a highly infected country—collective interventions are required as well.
Collective interventions are usually coordinated by government; they involve and affect everyone, though they may not be to everyone’s liking. These actions include: disinfecting public spaces, closing borders, restricting individuals’ movements, shutting schools, banning gatherings, closing businesses, instituting testing and contact tracing, quarantine of exposed individuals and issuing “stay at home” orders. Because they often impose hardships on the apparently uninfected, they are often resented and even resisted.
Another way to categorize interventions is by how they act as barriers to the spread of the virus. Some, like mask wearing, hand washing, sanitizing surfaces or erecting Plexiglas barriers, act by reducing person-to-person transmission of the virus. Others, like self-isolation, quarantine and school closing, reduce virus spread by reducing human contact.
None of these measure a mutually exclusive; in fact, they often have complementary strengths and weakness and work best in various combinations with each other. Each is a layer of defense, like those Swiss cheese slices and their “holes.” Two layers are good; four is better. Some layers are definitely better than others—widespread testing of everyone, masks and vaccines, but no single intervention is good enough.
Masks are enormously effective, despite all the misinformation about them. Let’s do the math. If a type of mask only stops 50% of virus transmission and is only worn by 50% of the people, it still has a tremendous impact. If you start with 100 cases of the virus and no one wears masks, at the end of one month you will have 31,280 cases. If only 50% of the people wear a mask that is only 50% effective, with the same initial 100 cases you will have only 584 cases at the end of the moth, a 98.1% reduction in cases!
To manage the major surge we are experiencing we need to implement a combination of interventions that: 1) reduce transmission and 2) limit contact between people. We need to implement not one or two interventions, but three or four or whatever is needed. An example of how not to do this is illustrated by the repeated White House outbreaks, including the President. This happened because they relied on a single intervention, testing, and not multiple simultaneous interventions, like requiring mask wearing. They also chose a single rapid test that was not very accurate, an ineffective intervention.
Every country around the world that has effectively managed COVID-19 has deployed this Swiss cheese strategy, using the particular interventions that made sense to them. South Korea relied on mask and widespread testing; New Zealand, an island nation, relied on border-closure and extensive contact tracing; Greece banned gatherings and closed schools. The key is to know what works best for your country and what you can effectively implement. Lockdowns reduce viral spread 81%, but they are devastating to the economy and impossible to sustain. Deploying multiple, less-damaging interventions is much less expensive and ultimately more effective.
We have the tools and the knowledge to manage the pandemic; we’ve had them all along. What we lacked was leadership and good management. What we need is leadership that helps people understand what is happening and models good behavior. This requires honest communication about the rationales for and the limitations of recommended policies. That, in turn, builds trust.
Successful management of the pandemic will lead to a more rapid recovery of the economy. The two are tied together, something the current administration never understood. If people are afraid for their lives or their loved ones, they are not going to engage in normal social interaction or their usual consumer behavior. Once people begin to believe the virus is on the wane the economy will normalize.