Thousands of hospital workers still unvaccinated
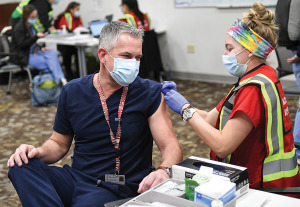
The clock is ticking for workers at large hospital systems across central Indiana to get vaccinated for COVID-19 or risk losing their jobs.
The clock is ticking for workers at large hospital systems across central Indiana to get vaccinated for COVID-19 or risk losing their jobs.
Ascension’s decision to require vaccinations follows similar mandates by all three other major health systems here.
Franciscan joins two other large hospital systems in central Indiana—Indiana University Health and Community Health Network—in laying down the new health requirement.
A new report submitted to the Indiana Legislative Council calls for the regulation of “white bagging,” a practice that requires hospitals to buy drugs from an outside pharmacy, which delivers them premixed ahead of time of the patient’s visit. It is a growing practice, aimed at lowering the cost of care, but many providers say it can compromise care.
The federal government issued rules Thursday to shield Americans from large, unexpected medical bills after patients wind up in emergency rooms or receive other care they did not realize lay outside their insurance networks.

Gil Peri begins his new job just as the system is about to undertake one of its biggest projects in a decade—relocating its maternity services from Methodist Hospital to new, centralized maternity and newborn health unit at Riley Hospital, as part of a $142 million expansion.

Indiana University Health has created a lab to testing the vulnerability of hundreds or even thousands of devices, to protect both patients and the hospital system’s records.
Legal experts say such vaccine requirements, particularly in a public health crisis, will probably continue to be upheld in court as long as employers provide reasonable exemptions, including for medical conditions or religious objections.
In a scathing ruling Saturday, U.S. District Judge Lynn Hughes of Houston deemed lead plaintiff Jennifer Bridges’ contention that the vaccines are “experimental and dangerous” to be false and otherwise irrelevant.
The hospital system’s CEO said Wednesday that no staff members have been terminated in relation to the patient’s care, which was a recommendation of an outside board that reviewed the case.

The heavy investment in the campus—including a new women’s hospital and a brain and spine center—is the latest indication that Ascension St. Vincent is committed to the location, a major anchor along the busy West 86th Street corridor.
The group, Hoosiers for Affordable Healthcare, is pushing an amendment that would require most of Indiana’s hospitals to hold annual public meetings to explain their prices, including any price increases, and to take questions about their finances.

Since July, however, the hospital system has seen an “upward positive trend in all its services,” it said in a debt filing, the latest signal that the worst of the pandemic’s financial affects on hospitals might be over.

Health care practitioners and insurers are fighting over the hefty prices hospitals charge for specialty drugs to treat patients with cancer, vision loss, low white-blood-cell count and other serious diseases.

A prominent Indianapolis surgeon is suing Indiana University and Indiana University Health, claiming they broke his contract and interfered with his ability to get another job.

Declines were seen almost across the board in patient service categories, including hospital admissions, surgeries, ER visits, radiological exams, due in part to a government order to shut down elective procedures for several months.
U.S. hospitals face up to $122 billion in lost revenue this year as the pandemic continues its rampage, threatening to push more critical-care centers into bankruptcy or out of business entirely.
The hospitals, including six in the Indianapolis area, will be docked millions of dollars by the Centers for Medicare & Medicaid Services for high rates of infection or patient injuries.

As hospitals and health departments scramble to erect temporary clinics, the big questions are how fast states can roll out the vaccines and how long it will take for people to get protected.
Vice President-elect Kamala Harris took up Dr. Moore’s cause on Tuesday, saying the complaints of Black women are “often downplаyed or ignored in our health care system.”